You chose a Medicare Part D plan. Now your needs change. You wonder, “Can you change Medicare Part D plan mid-year?” The short answer is mostly no, unless you qualify for a Special Enrollment Period (SEP). Read this blog to know all about medicare part d plans mid-year change.
What is a Medicare Part D Plan Change?
When you swap from one Medicare drug plan to another during the year, that’s a Medicare Part D plan change. It’s also called switching Medicare drug plans. You do this to get lower costs, better coverage, or fix gaps in your prescription coverage.
Changing Medicare plans outside open enrollment is tricky. Most people can only do it during certain windows.
Standard Times You Can Change Part D
You do have regular windows to change your Part D plan.
- Annual Open Enrollment (AEP): Oct. 15 – Dec. 7. During this period, you can join, drop, or switch plans. Changes take effect on January 1, 2023.
- Medicare Advantage Open Enrollment: Jan. 1 – Mar. 31. If you’re in a Medicare Advantage with drug coverage, you may shift to another MA plan (with or without a drug plan) or return to Original Medicare and get a Part D plan.
But outside those, you often can’t change, unless you hit a SEP.
Special Enrollment Periods (SEP): Your Way In Mid-Year

A Special Enrollment Period (SEP) is your mid-year escape hatch. It lets you change your Medicare Part D plan outside the usual windows if a qualifying event happens. Here are common SEP triggers:
- You move out of your plan’s service area.
- You lose other drug coverage (that was “creditable”), e.g., employer retiree plan ends.
- You enter, leave, or live in a nursing home/institution.
- Your Part D plan terminates or stops serving your area.
- You qualify for Extra Help / Low-Income Subsidy (LIS) or lose it. In that case, changes are allowed more often.
- A 5-Star Plan SEP: if a 5-star Part D plan is available in your area, you can join it once a year between Dec. 8 and Nov. 30.
Also, as of 2025, rules for dual eligibles and Extra Help have shifted. SEP frequency is now monthly for some. Each SEP has its own rules about when you can request a switch and when the new coverage begins.
| Switch Medicare Drug Plans During Your SEP Window PrimeLife helps you act fast and avoid losing prescription coverage. Enroll Now |
Who Can’t Change Mid-Year (Usually)
If you’re in Original Medicare with a standalone Part D plan, without meeting SEP triggers, you generally cannot change plans mid-year.
If you try, you’ll be denied until the next open season.
Also, the Medicare Advantage Open Enrollment does not let you change a stand-alone Part D plan if you’re in Original Medicare.
How SEP Changes Take Effect
When your SEP qualifies, here’s what happens:
- You submit the request (call 1-800-MEDICARE or use plan tools) to enroll in the new Part D.
- The old plan is automatically dropped when the new one begins. You don’t need to actively cancel.
- The effective date is often the first of the month following your request (or a designated date per SEP rules.
- For some SEPs (like Dual / Extra Help), because of rule changes, you may make changes monthly, but only certain types of changes are allowed.
Be careful: there is often a deadline window to act after a qualifying event (like within two months of your move).
| Don’t Miss Your Chance to Change Medicare Part D Talk to PrimeLife today and secure better drug coverage before it’s too late. Get Help |
What About Formularies & Mid-Year Drug Changes?
Even if you can’t change your plan, your plan may change which drugs it covers during the year. That’s about formulary changes.
- Part D plans can add or drop drugs during the year.
- If your drug is removed or moved to a higher cost tier, your plan must notify you (typically 60 days before the change) and give you options.
- If your drug is removed entirely and no alternatives exist, you may be allowed a drug transition or protection, or use your SEP rights, depending on the situation.
So, even if you can’t change plans mid-year, your prescription coverage changes might force you to consider switching when possible.
Why You’d Want to Change Mid-Year
Switching your Medicare Part D plan mid-year can help you:
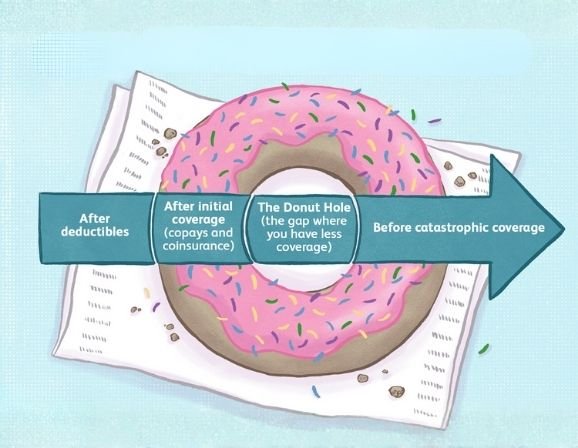
- Lower your drug costs (premiums, copays, tiers).
- Choose better formulary coverage for your medicines.
- Adjust if your health needs have shifted (you started new prescriptions).
- Avoid high out-of-pocket costs mid-year.
But since opportunities are limited, you must act fast when a SEP triggers.
How to Change: Step by Step (Mid-Year / SEP)
- Check if you qualify for SEP: review past events (move, lose coverage, LIS change).
- Compare current and new plans: use Medicare’s plan finder or broker.
- Enroll in new plan: call 1-800-MEDICARE or use your new plan’s enrollment tools.
- Let the new plan take effect: the old plan ends automatically.
- Confirm coverage & pharmacy acceptance: ensure your pharmacy and drugs are accepted under the new plan.
Pitfalls & What to Watch Out For
- Missing the SEP window: if you wait too long after a qualifying event, you lose your chance.
- Gaps in coverage: switching mid-year might cause small gaps if effective dates misalign.
- Penalties: if you went without creditable coverage for 63+ days before switching, a late enrollment penalty may apply.
- Plan restrictions under new rules: Some SEPs allow only limited types of changes, especially under 2025 SEP changes.
- Formulary surprises: even in your new plan, drugs may move tiers or be removed later.
Final Thoughts
You can’t freely change Medicare Part D plans mid-year, only under Special Enrollment Periods triggered by life events. Outside of open enrollment, your chance to switch depends on qualifying for SEP. Plans also may change their drug coverage (formularies) mid-year, which sometimes forces adjustments.
If your drug needs, coverage area, or subsidy status changes, check SEP rules and act quickly.
FAQs
Can Medicare Part D be changed anytime?
No. You can only change during open enrollment or a Special Enrollment Period triggered by a qualifying event.
Can I change my Medicare plan in the middle of the year?
Yes, but only if you qualify for SEP (for example, you moved or lost other coverage).
Is there a penalty for switching Medicare plans?
Not for switching itself. But if you had a long gap without creditable drug coverage, a late enrollment penalty may apply to your premium.
Is it too late to change the Medicare plan for 2025?
If you’re outside AEP and don’t qualify for SEP, yes, your next chance is during Oct. 15–Dec. 7, unless your life event triggers an SEP now.