If you miss signing up for Medicare prescription drug coverage when you first become eligible, you may face the Medicare Part D penalty. This fee isn’t a one-time charge, it sticks with you as long as you have Medicare drug coverage. Understanding how it works helps you avoid paying extra every month for something that could have been prevented.
What Is the Medicare Part D Penalty?
The Medicare Part D penalty is an added cost to your monthly drug plan premium if you didn’t sign up for Part D when you were first eligible. It’s Medicare’s way of encouraging timely enrollment so everyone contributes fairly to the drug coverage system.
This penalty starts small but grows with time. The longer you go without drug coverage, the higher your penalty becomes.
The penalty applies only if:
- You went 63 or more consecutive days without creditable prescription drug coverage.
- You didn’t have other drug coverage that was at least as good as Medicare’s standard plan.
When the Medicare Penalty Applies
Medicare gives everyone a window to join a prescription plan. If you miss it, the clock starts ticking on your late enrollment penalty.
Here’s when it applies:
- You didn’t sign up for Part D during your Initial Enrollment Period (IEP).
- You didn’t have creditable coverage, meaning drug coverage that meets or exceeds Medicare’s standard.
- You go 63 continuous days without any drug coverage.
That 63-day mark is critical. Once you cross it, Medicare considers you uncovered, and the penalty automatically adds up once you finally enroll.
Late Enrollment Penalty Calculation
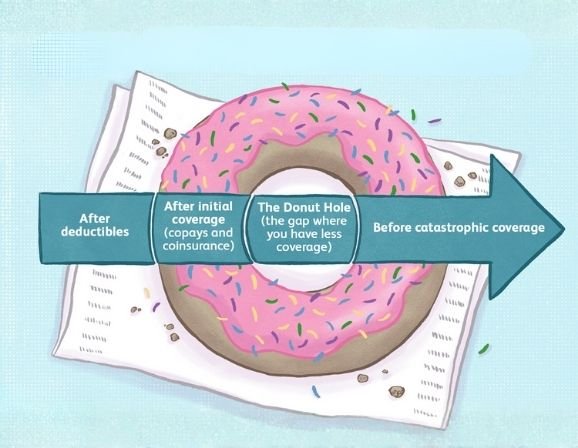
The late enrollment penalty calculation is straightforward but strict. Medicare calculates your penalty based on how long you went without coverage and a national base premium that changes each year.
Here’s the formula:
1% of the national base premium × number of uncovered months = monthly penalty.
Example:
If the national base premium is $35 and you went 10 months without coverage, your penalty is $3.50 (1% × 10 × $35). This amount is added to your monthly premium every month, permanently.
Medicare rounds your penalty to the nearest $0.10, and because the base premium changes annually, your penalty may also slightly change each year.
| Avoid Costly Delays in Medicare Enrollment Get help signing up for Medicare Part D on time with Prime Life Financial’s experts. Enroll Now |
How to Avoid Medicare Part D Penalty

Avoiding the penalty starts with understanding your timeline. Medicare offers a seven-month Initial Enrollment Period, starting three months before your 65th birthday and ending three months after.
Ways to avoid the penalty:
- Enroll in Part D as soon as you’re eligible.
- Keep creditable prescription drug coverage if you’re covered under an employer or union plan.
- Don’t go 63 or more days without drug coverage.
If you already have employer or union coverage, confirm it’s “creditable” each year, your employer should send a notice. Keep that document as proof in case Medicare questions your coverage later.
Medicare Part D Late Enrollment Rules
Medicare has specific late enrollment rules that decide when and how the penalty applies. These include your eligibility date, whether you had creditable coverage, and how long you went without it.
Here’s how it usually works:
- If you miss your initial enrollment and don’t qualify for special enrollment, you’ll have to wait until the Annual Enrollment Period (October 15 to December 7).
- Your penalty will then start when your new coverage begins in January.
- The penalty stays for as long as you have Medicare Part D.
| Enroll Before the Deadline Medicare Part D enrollment ends December 7. Don’t wait to avoid penalties and higher premiums. Join Today |
Part D Penalty Appeal Process
If you believe your penalty was assigned in error, you have the right to appeal. Medicare calls this the Part D penalty appeal process.
Here’s what to do:
- Wait for your plan to send you a letter explaining your penalty.
- File a reconsideration request with Medicare.
- Include documentation proving you had creditable coverage (for example, a notice from your employer).
You must submit the appeal within 60 days of receiving your penalty notice. While the appeal is being reviewed, you still pay the penalty amount, but you may get a refund if Medicare overturns the decision.
Why Creditable Prescription Drug Coverage Matters

Creditable prescription drug coverage means your plan’s benefits are at least equal to Medicare’s standard drug coverage. It protects you from late penalties if you delay enrolling in Part D.
Typical examples include:
- Employer or union health plans
- TRICARE or VA drug coverage
- Certain retiree or federal employee health plans
If you’re unsure whether your coverage counts as creditable, always check with your benefits provider or contact Medicare directly.
Why the Penalty Exists
The penalty may seem unfair, but it helps keep drug coverage affordable for everyone. Without it, some people would delay joining until they needed expensive medications, driving up costs for all beneficiaries.
By enrolling on time, you help maintain stability in the Medicare system and avoid paying extra fees down the road.
The Real Cost of Delay
Going just one year without coverage could add hundreds of dollars to your annual health costs. For many seniors on fixed incomes, that’s a preventable burden. Once added, the penalty doesn’t go away, it follows you for as long as you have Part D. Timely enrollment is not just a financial choice; it’s peace of mind.
| Secure Your Medicare Coverage Today Don’t let penalties reduce your savings. Prime Life Financial can help you enroll on time. Get Started |
Timing Is Everything with Part D
Avoiding the Medicare Part D penalty is about staying proactive. Know your enrollment window, confirm your coverage is creditable, and enroll before the 63-day rule catches you off guard.
Prime Life Financial helps simplify the process, ensuring your drug coverage starts on time, without unnecessary penalties. Act early, stay covered, and keep your healthcare costs under control.
FAQs
What is the Medicare Part D late enrollment penalty?
It’s an ongoing monthly fee added to your drug plan premium when you delay enrollment without creditable coverage for 63 days or more.
How do I get my Part D penalty waived?
You can appeal the penalty by proving you had creditable prescription drug coverage during the time you were uninsured.
How to avoid Medicare late enrollment penalties?
Sign up during your Initial Enrollment Period or keep creditable coverage under an employer or union plan.
What is the 63-day rule for Medicare Part D?
It’s the limit on how long you can go without drug coverage. After 63 days, Medicare begins adding penalties once you enroll.
References: Avoid late enrollment penalties. (n.d.). Medicare. https://www.medicare.gov/basics/costs/medicare-costs/avoid-penalties