Choosing the right Medicare drug plan can feel confusing, especially when it comes to the Medicare Part D deductible. Many people ask, “What does this number mean, and how much will I really pay before my plan helps?” The deductible is the first step in understanding your total prescription drug costs.
In this guide, we’ll break down how the deductible works, how it connects to other phases like copayments and out-of-pocket caps, and why the new 2025 changes make it easier to plan your budget.
What Is a Medicare Part D Deductible?
When your Medicare drug plan has a Medicare Part D deductible, it means you must pay a fixed amount first before the plan starts sharing costs.
You pay the full cost of covered drugs (that apply to the deductible) until you reach that amount. Not all drugs may count toward it, some plans waive the deductible for generics or certain tiers.
| The Medicare Annual Enrollment Period Runs from October 15 to December 7. Use PrimeLife to compare plans & ensure you pick one with a reasonable Medicare Part D deductible today. |
How the Deductible Fits with Medicare Part D Costs

Your total Part D costs include several pieces:
- The deductible
- Copayments or coinsurance
- The monthly premium
- Any extra charges (e.g., from income)
A plan might have a deductible up to a federal limit. In 2025, many plans have $0 deductible, but some still use the full limit.
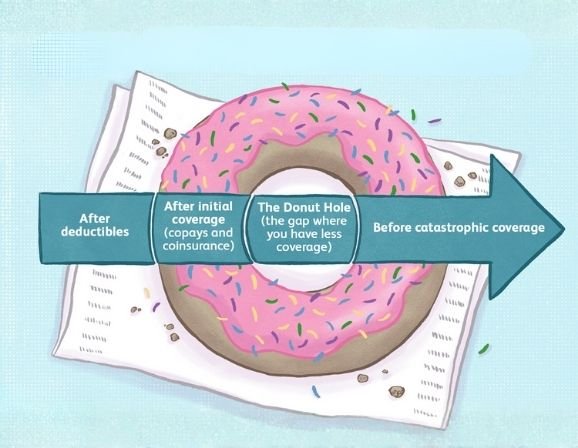
The Inflation Reduction Act removed the traditional “donut hole” phase and capped out-of-pocket costs. Before your deductible is met, you pay full costs (for qualifying drugs). After that, you move into the initial coverage phase.
| Thinking About Switching Part D Plans? PrimeLife can model your Medicare Part D costs (deductible + copays) so you can pick the best fit now. Contact Now |
Initial Coverage Phase: After Deductible
Once you meet your deductible, you enter the initial coverage phase.
In this phase, you pay a share (copay or coinsurance) of the drug cost, and the plan pays the rest, up to a threshold.
- Some drugs will require a fixed copayment (for example, $5 for generics).
- Other drugs require coinsurance, like paying 25% of the cost.
- The plan’s formulary (drug list) and tiers affect what you pay.
| Don’t Wait Until You Need a Drug. Contact PrimeLife early so you understand your Medicare Part D copayments and coinsurance under initial coverage. Contact Today |
Copayments & Coinsurance in Part D
Copayment (copay) = a flat fee you pay (e.g. $10) for a drug.
Coinsurance = a percentage of the drug cost (e.g. 20%).
What you pay depends on:
- The drug’s tier (generic, brand, specialty)
- Whether the drug is on your plan’s formulary
- Whether the plan has waived the deductible for that tier
Before deductible: you pay full cost (if that drug tier counts toward deductible).
After deductible: pay copay or coinsurance, depending on drug tier.
Out-of-Pocket Cap & Changes in 2025
A big change in 2025: your maximum out-of-pocket drug costs are capped at $2,000 (this excludes premiums).
That means once you hit $2,000 in eligible drug spending, you pay $0 for covered drugs the rest of the year (for those drugs).
Also:
- The standard deductible limit is rising (it may go to $615 in 2026).
- The “donut hole” or coverage gap is essentially eliminated, so cost sharing is smoother.
What Happens When You Meet the Deductible?

When your deductible is met, your plan starts to pay its share for many (not necessarily all) covered drugs.
You shift from full cost to copayment/coinsurance as defined by your plan’s design.
If you reach the out-of-pocket cap, pay zero for covered prescriptions.
- Drugs not covered by the plan or in excluded tiers may still require full cost.
- Some plans exclude a deductible for certain tiers (e.g., generics may skip the deductible).
- After cap, your cost is $0 for eligible drugs.
Tips for Managing Prescription Drug Costs
- Choose a Part D plan with a low or $0 deductible if possible.
- Use lower-tier drugs (generics) when effective.
- Check if a plan waives the deductible for certain tiers.
- Keep an eye on spending so you don’t overshoot your cap.
- If your income is limited, apply for Extra Help (helps with premiums, deductibles, copays)
- Enroll in Part D when first eligible to avoid late penalties.
- Re-evaluate your plan yearly during Open Enrollment (Oct 15–Dec 7).
- Prime Life can model costs across drugs and plans to help pick the best one.
Final Thoughts
The Medicare Part D deductible is more than just a number, it sets the stage for every other cost you’ll pay during the year. Once you understand how it works with copays, coinsurance, and the new out-of-pocket cap, you can make smarter choices and avoid surprises at the pharmacy.
With the 2025 updates, Medicare drug coverage is becoming more predictable, but comparing plans is still critical. Prime Life can help you review options, project your yearly costs, and enroll in a plan that keeps your medications affordable. Don’t wait, Annual Enrollment runs Oct 15 through Dec 7.
FAQs
How does the Medicare Part D deductible work?
You must pay a fixed amount out of pocket for covered drugs before your drug plan’s cost-sharing begins. After the deductible is satisfied, you pay copays or coinsurance.
How does the Medicare Part D cap work?
In 2025, once your total eligible drug costs reach $2,000, you pay $0 for covered prescriptions for the rest of the year (excluding premiums).
What is the maximum out-of-pocket for Medicare Part D?
As of 2025, the cap is $2,000. After that, you have no further drug costs (apart from premiums) for covered drugs.
What happens when I meet my Medicare deductible?
Your plan switches from you paying full cost to paying cost share (copays/coinsurance). Then once you hit the out-of-pocket cap, your cost becomes zero for covered drugs.
References
How much does Medicare drug coverage cost? (n.d.). Medicare. https://www.medicare.gov/health-drug-plans/part-d/basics/costsOmdahl, D. (2021, March 9). Making sense of the Medicare Part D Drug Plan deductible. Forbes. https://www.forbes.com/sites/dianeomdahl/2021/03/09/making-sense-of-the-medicare-part-d-drug-plan-deductible/